THE ROLE OF
OMEGA-3 FATTY ACIDS
IN PATIENTS WITH
NON-ALCOHOLIC FATTY
LIVER DISEASE*
OMEGAs

Non-alcoholic fatty liver disease NAFLD is considered to be a liver manifestation of metabolic syndrome. The high prevalence of NAFLD in western countries correlates with the high prevalence of overweight and obesity. Since there is currently no standardized pharmacological treatment, there is an increased interest in nutritional interventions for prevention and treatment of NAFLD. Omega-3 fatty acid supplementation may have beneficial effects in regulating hepatic lipid metabolism, inflammation and adipose tissue function. Special attention should be given to krill oil because of high bioavailability and ability to reach target tissues.
Non-alcoholic fatty liver disease (NAFLD) is defined as an excess accumulation of fat in the liver, unconnected with alcohol intake, and is the leading cause of chronic liver diseases in the world. NAFLD is considered to be the most prevalent cause of liver failure due to the increase in the prevalence of obesity in the world (1). The exact global prevalence of NAFLD is unknown, but it is estimated that it affects 10%-24% of the world population. This proportion is significantly higher in western countries, where it amounts to 20%-40% of the population, with 20%-30% in Europe (2).
It has been shown that central obesity is a significant risk factor for NAFLD, even in persons with normal body mass index (BMI). Generally, NAFLD is considered as a liver manifestation of metabolic syndrome and the key role in its pathogenesis plays insulin resistance (3). The onset and progression of NAFLD is attributed to a number of factors that are part of the theory of “multiple hits”, which indicates that NAFLD is a result of liver inflammation caused by numerous intestinal triggers and those associated with fatty tissue (1,4). There is currently no standardized pharmacological treatment and the only proven effective therapeutic strategy is lifestyle modification, therefore it is important to determine the potential dietary targets and nutritional interventions for prevention and treatment of NAFLD (5).
INTRODUCTION
Omega-3 fatty acid treatment may have beneficial effects in regulating hepatic lipid metabolism, inflammation and adipose tissue function. Recent studies and meta-analyses indicate that effects of fish oil omega-3 fatty acids in NAFLD are showing promise and suggesting that these fatty acids may be useful in the treatment of NAFLD (6). Nevertheless, krill oil as a form of highly bioavailable phospholipid omega-3 naturally containing astaxanthin and choline has not been extensively studied in humans. Several animal studies done with krill oil have shown that it suppresses hepatic steatosis, therefore there is a great potential of use of krill oil in patients with NAFLD (7).
The omega-3 index represents the sum of the masses of the two beneficial omega-3 fatty acids in erythrocyte membranes, eicosapentaenoic and docosahexaenoic acids (EPA + DHA), and is expressed as a percentage in total fatty acids. In 2004, the index was proposed by Harris and von Schacky as a biomarker of cardiovascular risk of death (8). The analytical method commonly used to determine the omega-3 index in erythrocytes is gas chromatography, which is done after the fatty acid methylation procedure.
The choice to measure omega-3 fatty acid composition in erythrocyte membranes (rather than in the plasma, for example) is based on the fact that the effects of omega-3 fatty acids originate from their primary action at the level of cell membranes. Thanks to the erythrocyte survival in the circulation lasting 120 days, the omega-3 index is a long-term biomarker of omega-3 fatty acid intake that is unaffected by recently consumed foods. Furthermore, omega-3 index is considered to be a marker of cardiometabolic risk (9).
THE ROLE OF OMEGA-3 FATTY ACIDS AND OMEGA-3 INDEX
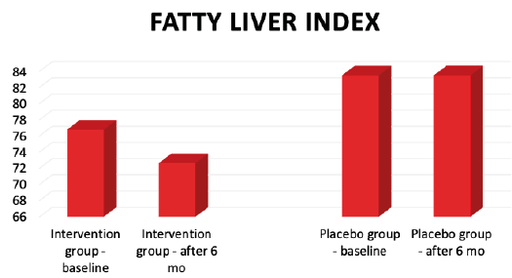
Figure 1. Fatty liver index in the intervention group and in the placebo group at the baseline and after 6 months of the study.
Nutrition plays an important role in the management of NAFLD. Studies show that NAFLD patients are more likely to consume energy-rich foods, saturated and omega-6 fatty acids, cholesterol, and sweetened beverages, while not eating enough fresh fruits, green vegetables, fiber, and omega-3 fatty acids (10). Numerous studies, including the prominent PREDIMED study, support the thesis that the Mediterranean diet is associated with a lower prevalence of NAFLD (11).
Therefore, as part of the NAFLD diet, a Mediterranean diet rich in single and omega-3 unsaturated fatty acids, fiber, complex carbohydrates, micronutrients and polyphenols and many other biologically active compounds is recommended. Specific restrictions apply to fructose and simple carbohydrates, whose intake should be retained in 10% of total energy intake. Furthermore, weight loss of 7% or more, with proper nutrition for at least one year, may improve liver histology in patients with NASH and NAFLD. Mediterranean diet, therefore has verified beneficial effects on the liver and cardiometabolic factors, as well as weight reduction (12). The beneficial effect of the Mediterranean diet is linked to the improvement of cardiometabolic status (lowering serum triglycerides and glycemic control) and the antioxidant effect of the components of the Mediterranean diet (polyphenols and vitamin E), thereby reducing oxidative stress crucial for the development of insulin resistance (13).
Some isolated pharmacologically active nutrients are being investigated as a potential aid to NAFLD, in particular vitamin E, vitamin D, probiotics and omega-3 fatty acids. Studies suggest a direct role for vitamin D in modulating liver inflammation and fibrosis onset as well as improving the hepatic response to insulin. However, further randomized, placebo-controlled studies are needed to determine appropriate doses and efficacy of vitamin D. Changes in the composition of the gut microbiota are observed in patients with NAFLD (14, 15). Several mechanisms for the interaction of the gut microbiome and NAFLD have been proposed, including dysbiosis-induced intestinal endothelial barrier dysregulation and consequent translocation of bacterial components leading to inflammatory changes in the liver. Furthermore, numerous metabolites produced by the gut microbiota (including small doses of alcohol) can affect the liver and susceptibility to NAFLD.
Therefore, manipulation of the gut microbiome composition by probiotics, prebiotics, postbiotics or synbiotics has proven to be desirable in order to improve the liver phenotype in patients with NAFLD (16).
Omega-3 fatty acids, EPA and DHA, have beneficial effects in regulating the lipid metabolic pathways in the liver, hepatic lipogenesis, adipose tissue function, inflammation and lowering triglyceride accumulation in the liver by reducing the gene expression of several transcription factors involved in lipogenesis and triglyceride accumulation (6). Mechanistic effect of omega-3 fatty acids on liver steatosis is based on downregulation of sterol-regulatory-element-binding protein 1c (SREBP-1c) and upregulation of peroxisome–proliferator-activated receptor α (PPAR-α). Those mechanisms promote fatty acid oxidation and reduce steatosis (17). Furthermore, omega-3 fatty acids increase synthesis of resolvins, molecules with anti-inflammatory effects (18). Results of a meta-analysis that examined the effect of omega-3 fatty acids in the treatment of NAFLDs, support their beneficial effect in optimizing liver steatosis, liver enzymes, and blood lipid levels (triglycerides and HDL), in which they may slow the progress of NAFLD (19).
Omega-3 index is a promising biomarker for cardiovascular morbidity and mortality and therefore may be a useful indicator of NAFLD risk. Although Parker et. al. (20) did not find the Omega-3 Index to be predictive of fatty liver in the group of eighty overweight adults, the evidence linking NAFLD with low n-3 PUFA (intake and status) is strong.
LIFESTYLE CHANGES IN THE THERAPY OF NAFLD
Considering that NAFLD patients have a higher risk of developing cardiovascular disease, the aim of our pilot study conducted in years 2016 and 2017 was to examine the influence of omega-3 fatty acids from krill oil combined with selenium and vitamin E on various risk factors in NAFLD patients.
The study was randomized, double blind and placebo controlled, and lasted for 6 months. It included 14 NAFLD patients, ages 39 to 64, divided into two groups. In the intervention group, subjects consumed krill oil capsules (Almagea® KRILL OIL+ containing 1500 mg krill oil, 36 mg vitamin E, 165 mcg selenium daily), while in the placebo group subjects consumed soybean oil capsules (1500 mg soybean oil daily). The patients were diagnosed with NAFLD during the year 2017 by the standard diagnostic algorithm procedure and tools including ultrasound. Further clinical evaluation excluded other liver diseases such as viral and drug induced hepatitis, hemochromatosis, autoimmune liver diseases, Wilson’s disease, malignant disease, liver cirrhosis and alcoholic liver disease (defined as intake of >40 g/day of alcohol for men and >20 g/day of alcohol for women). Blood sample analyzes were performed in the competent medical-biochemical laboratories and in the medical-biochemical laboratory of the University Hospital Centre Zagreb. Methods included standard anthropometric measurements, serum lipids, liver enzymes, the value of fatty liver index (FLI) as well as omega-3 index according to method by Rose and Oklander and ISO method 5509. The results of the study showed that there was a statistically significant reduction in body mass (p= 0.028), BMI (p= 0.043) and waist circumference (p= 0.041) in the intervention group compared to the placebo group where the change was not statistically significant.
None of the groups showed statistically significant changes in serum lipids and liver enzymes. Fatty liver index decreased in intervention study in 75% patients with NAFLD, while in placebo group, FLI increased in 66 % of the subjects.
Results of assessment of cardiovascular risk before the intervention are indicating insufficient cardio-protection in both groups because of low omega-3 index: 3,25 ± 1,14 % in females and 3,74 ± 0,97 % in males. After the intervention, there was a 7,7% increase in omega-3 index in the intervention group, while there was 6% decrease in omega-3 index in placebo group.
These results indicate the potential of use of krill oil in the group of NAFLD patients (21). Considering that this is the first research on this subject, further studies should involve a larger number of NAFLD patients that would establish the dose of krill oil omega-3 fatty acids as a treatment and determine the preferable duration of therapy. Furthermore, compliance should be closely monitored, as well as lifestyle and diet changes during the study by a weekly phone call and periodic control visits to the hospital. Since the NAFLD is a cluster of clinical features, the approach of synergistic application of protective nutrients could also be taken into consideration by simultaneous provision of several nutrients – omega-3 fatty acids, antioxidant nutrients, vitamin D and probiotic bacteria as well as lifestyle changes.
OUR EXPERIENCE WITH USE OF KRILL OIL IN PATIENTS WITH NAFLD
*Article previously published in Agro Food Industry Hi Tech 31(3) 2021.
DARIJA VRANEŠIĆ BENDER
University Hospital Centre Zagreb | Croatia
Bio...
Prof. Darija Vranešić Bender, BSc, PhD is the head of nutritional consulting company Vitaminoteka based in Croatia, and works as a clinical nutritionist at the University Hospital Zagreb, Unit of Clinical Nutrition. She is Professor at the University of Zagreb, where she teaches diet therapy and clinical nutrition. She is skilled in clinical nutrition and clinical use of dietary supplements, participated in many scientific and educational projects and member of several international organizations and scientific boards.





